AN INTERESTING CASE OF 32 YEAR OLD FEMALE WITH DIFFICULT SPEECH AND RECENT ONSET FACIAL PUFFINESS
-Pain and burning sensations over the upper back for 7 years
-Breathlessness on exertion for 7 years
-Difficulty in speech for 5 years
-Facial puffiness since 2 weeks
She was apparently asymptomatic 7 years back, then she developed pain in the back,scapular region, dragging type a/w burning sensations.
She says she started having breathlessness on exertion(even on climbing stairs/walking for a distance of 1/2-1km) since 7 years.
She says all her problems started since her last childbirth 7 years ago when she had postpartum hemorrhage and hysterectomy done for it.
History of bilateral swelling of both the legs since 7 years.
History of Paresthesias of both upper and lower limbs since 7 years.
History of muscle cramps in both the calfs since 7 years.
She says she developed difficulty in speech i.e slowness in speech,exhaustion on talking for sometime, stuttering, insidious onset, gradually progressive and of 5 years duration(2 years after her last delivery).
She gives history of loss of appetite, Indigestion, Hiccoughs, Easy fatiguability,Abdominal bloating after intake of food,all these symptoms since her last childbirth.
She developed Facial puffiness since 2 weeks, after having started on steroids and DHEA by a local doctor for cause unknown to the patient(No documentation available as to why steroids were started).
History of Diffuse chest pain,pricking type-Pins and needles,increases on respiration since 15days not a/w palpitations/giddiness.
History of dryness of mouth and difficulty in swallowing, aggravated over the last one week.
History of easy fatiguability present.
History of cold intolerance present.
History of constipation present.
History of excessive sleep present.
History of excessive loss of hair present.
No history of orthopnea/PND.
No history of increased thirst/polyuria/polyphagia.
No history of loss of concentration/memory problems/blurring of vision/headache/depression/weight gain/seizures.
Menstrual history-
She attained her menarche when she was 14 yrs old and had regular 28-30 day cycles.She bleeds for 3 days with moderate flow and change of about 2-3 pads per day not a/w any dysmenorrhoea/passage of clots.
Marital history-
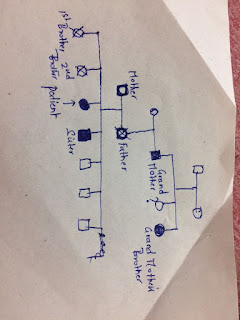
She got married when she was 15 yrs old and it was a non consanguineous marriage.
Obstetric history-
She delivered a healthy female baby through NVD when she was 16 yrs old. The female baby is now 16yrs old and is doing well. The baby was breast fed for an year and then stopped as she got pregnant again. At the time of her first pregnancy the patient was asked to take ?anti D antibodies in v/o Rh negative pregnancy but she dint.
She is an O negative female.
She got pregnant again the 2nd time,This time at 8th month of GA an emergency LSCS was performed in v/o IUD and she delivered a dead female baby.She was advised for Hysterectomy at this point but they denied for it. About 2 units of blood were transfused as the bleeding dint stop as narrated by the patient.Lactation was suppressed with medication.
She got pregnant the 3rd time 3 yrs after her 2nd pregnancy, but got aborted at 3rd month in v/o fetal anomalies.This time an induction of labour was done.
She then had her last pregnancy i.e 4th pregnancy 7 yrs back which was a complicated pregnancy. She was given Anti D antibodies at 7th month and she delivered a healthy male baby through LSCS at 9th month. LSCS was done as there was premature rupture of membranes and then after LSCS she was hysterectomised as bleeding dint stop- Possible Postpartum hemorrhage. She was transfused with 7 units of blood. She developed generalised edema as said by the patient for which she was treated and then all the sympyoms mentioned in the history of presenting illness started thereafter.
In her last pregnancy there was lactation failure, so her male baby was formula fed.
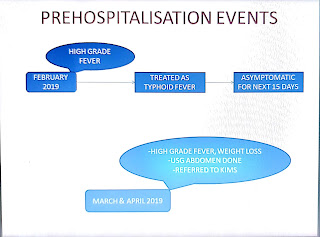
With these symptoms she consulted a local doctor who suspected hypothyroidism and got thyroid profile done which was normal. Then recently 2 weeks back they consulted another doctor who did few tests and started her on steroids and DHEA.
Personal history-
Mixed diet.
Loss of appetite present.
Bladder regular.
Bowel irregular-Constipation present-Once in 2 days and defecates hard stools not a.w any blood/pain/mucus-Fecal pellets
Sleep disturbances over last 1 week. Before that she used to have sleep excessively-increased sleepiness since her last childbirth.
No addictions/allergies.
General physical examination-
Patient is conscious and oriented.
Pallor +
Pedal edema, grade II upto knees,pitting type
No icterus/cyanosis/clubbing/koilonychia
Extensively dry skin seen.
Sparse hair over the body.
Hypopigmentation of perioral region.
Vitals-
Temp-98F
Pulse- 60 bpm,regular on right radial artery,Low volume.
No radioradial delay
Blood pressure- 90/60mmhg in supine posture on right arm
RR-14cpm
General systemic examination-
HIgher intellectual functions intact.
Cranial nerve examination normal.
Motor system-
Tone-Normal in both upper and lower limbs.
Power-5/5 in upper and lower limbs.
DTRs-Delayed relaxation of knee reflex seen
Sensory system-Normal
Cerebellar system-Normal
CVS-S1S2 heard,No murmurs.
RS-BAE+,Normal vesicular breath sounds heard.
Per abdomen- Soft, Tender in right iliac fossa on deep palption,Bowel sounds heard.







Comments
Post a Comment