Thesis case-T2DM with LEFT LOWER LIMB CELLULITIS.
A 47 year old male patient, shopkeeper by occupation and resident of nalgonda presented in the casuality with the chief complaints of
-Fever for 2 days
-Bleeding per rectum for 2 days.
He was apparently asymptomatic 2 days back, then he developed fever, of high grade, a/w chills and rigors, headache and intermittent in nature.
He gave history of bleeding per rectum,frank blood on the sqatting pan,not a/w any pain while defecation.
He had Pain abdomen in the periumbilical region,squeezing before passing stools and subsides after thet.
History of loose stools for 2 days,watery in consistency and 4-5 times per day.
History of giddiness present.
No history of nausea/vomitimgs/giddiness/burning micturition/cough/sore throat/generalised body pains/breathlessness.
Past history-
No history of similar complaints in the past.
He is known case of type2 diabetes mellitus since 4 years and on regular medication(Tab.Metformin 500mg and Glimeperide 1mg once daily).
Not a k/c/oHypertension/Thyroid disorders/Asthma/CVA/CAD/Epilepsy.
No history of any surgeries in the past.
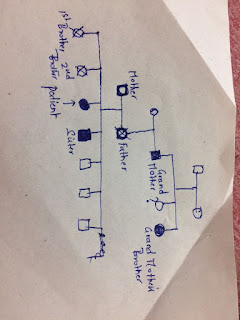
Family history-
No history of similar complaints in the family.
Mother is also a known diabetic since 10years.
No history of Hypertension/Thyroid disorders/Asthma/CVA/CAD/Epilepsy.
Personal history-
Mixed diet.
Appetite normal.
Bowel and bladder regular.
No sleep disturbances.
No addictions.
Occasional alcoholic.
Non smoker.
General examination-
Patient is conscious and oriented.
Pallor+
No icterus/cyanosis/clubbing/koilonychis/lymphadenopathy.
O/e Swelling of left lower limb is noticed and local rise of temperature was felt-Mild tenderness present.
Pedal edema upto the left knee,pitting type.
Right lower limb was normal.
Weight-75kgs
Height-160cms
WC-102cms
Waist-Height ratio- 0.64
Vitals-
Temp-100F in the first 2 days of admission and then he was afberile.
PR-96bpm,regular on right radial artery.
BP-120/70mmhg in supine posture on right arm.
90/70mhg in standing posture on right arm.
Postural drop was present.
Cardiovascular system-S1S2 heard,No murmurs.
Chest-Bilateral air entry present, Normal vesicular breath sounds heard.
Per abdomen-Soft, Non tender
No organmegaly.
Bowel sounds heard(3-4/min)
CNS-HMF intact.
No focal neurological deficit.
FUNDOSCOPY-No changes of diabetic retinopathy seen.
Provisional diagnosis-FEVER UNDER EVALUATION-?VIRAL PYREXIA WITH TYPE2DM WITH ?LEFT LOWER LIMB CELLULITIS.
Further evaluation was done and treatment was started.
INVESTIGATIONS-
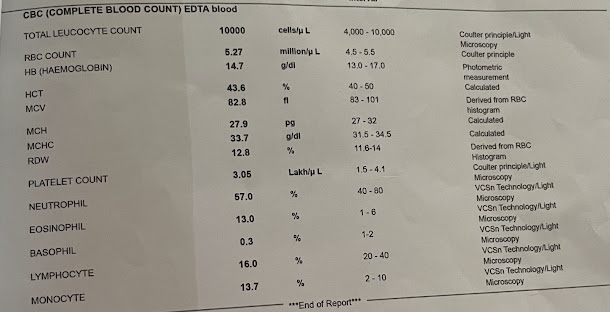
Complete blood picture-
Hb-10.0gm%(there was a drop of hb to 7.8 on the next day and postural drop was present-One unit of PCV was transfused in concern of any internal bleed-?Possible upper GI bleed)
TLC- 4700 cells/cumm
Platelets- Initially 1 lakh, f/b drop to 80000 and then a rise to 1.7 lakhs cells/cumm.
PCV-25.2vol%.
CUE
Albumin-Nil
Sugars-Nil
Pus cells-(2-3)
Epithelial cells(1-2)
Renal function tests were within normal limits.
Viral markers were negative.
Liver function tests were within normal limits.
Dengue serology was negative
PT-14 seconds.
INR- 1.0
Peripheral smear-Normocytic/hypochromic anemia with WBC within normal limits with adequate platelets.
Colour doppler of left lower limb- Minimal edematous changes noted below the knee s/o possible lower limb cellulitis.
Ultrasound abdomen-
Features s/o Cholecystitis was seen.
Mild ascitis.
ECG-Normal study.
Blood group-O positive.
He was treated as a case of Viral pyrexia with thrombocytopenia with serositis with T2DM with left lower limb cellulitis.
-Fever for 2 days
-Bleeding per rectum for 2 days.
He was apparently asymptomatic 2 days back, then he developed fever, of high grade, a/w chills and rigors, headache and intermittent in nature.
He gave history of bleeding per rectum,frank blood on the sqatting pan,not a/w any pain while defecation.
He had Pain abdomen in the periumbilical region,squeezing before passing stools and subsides after thet.
History of loose stools for 2 days,watery in consistency and 4-5 times per day.
History of giddiness present.
No history of nausea/vomitimgs/giddiness/burning micturition/cough/sore throat/generalised body pains/breathlessness.
Past history-
No history of similar complaints in the past.
He is known case of type2 diabetes mellitus since 4 years and on regular medication(Tab.Metformin 500mg and Glimeperide 1mg once daily).
Not a k/c/oHypertension/Thyroid disorders/Asthma/CVA/CAD/Epilepsy.
No history of any surgeries in the past.
Family history-
No history of similar complaints in the family.
Mother is also a known diabetic since 10years.
No history of Hypertension/Thyroid disorders/Asthma/CVA/CAD/Epilepsy.
Personal history-
Mixed diet.
Appetite normal.
Bowel and bladder regular.
No sleep disturbances.
No addictions.
Occasional alcoholic.
Non smoker.
General examination-
Patient is conscious and oriented.
Pallor+
No icterus/cyanosis/clubbing/koilonychis/lymphadenopathy.
O/e Swelling of left lower limb is noticed and local rise of temperature was felt-Mild tenderness present.
Pedal edema upto the left knee,pitting type.
Right lower limb was normal.
Weight-75kgs
Height-160cms
WC-102cms
Waist-Height ratio- 0.64
Vitals-
Temp-100F in the first 2 days of admission and then he was afberile.
PR-96bpm,regular on right radial artery.
BP-120/70mmhg in supine posture on right arm.
90/70mhg in standing posture on right arm.
Postural drop was present.
Cardiovascular system-S1S2 heard,No murmurs.
Chest-Bilateral air entry present, Normal vesicular breath sounds heard.
Per abdomen-Soft, Non tender
No organmegaly.
Bowel sounds heard(3-4/min)
CNS-HMF intact.
No focal neurological deficit.
FUNDOSCOPY-No changes of diabetic retinopathy seen.
Provisional diagnosis-FEVER UNDER EVALUATION-?VIRAL PYREXIA WITH TYPE2DM WITH ?LEFT LOWER LIMB CELLULITIS.
Further evaluation was done and treatment was started.
INVESTIGATIONS-
Complete blood picture-
Hb-10.0gm%(there was a drop of hb to 7.8 on the next day and postural drop was present-One unit of PCV was transfused in concern of any internal bleed-?Possible upper GI bleed)
TLC- 4700 cells/cumm
Platelets- Initially 1 lakh, f/b drop to 80000 and then a rise to 1.7 lakhs cells/cumm.
PCV-25.2vol%.
CUE
Albumin-Nil
Sugars-Nil
Pus cells-(2-3)
Epithelial cells(1-2)
Renal function tests were within normal limits.
Viral markers were negative.
Liver function tests were within normal limits.
Dengue serology was negative
PT-14 seconds.
INR- 1.0
Peripheral smear-Normocytic/hypochromic anemia with WBC within normal limits with adequate platelets.
Colour doppler of left lower limb- Minimal edematous changes noted below the knee s/o possible lower limb cellulitis.
Ultrasound abdomen-
Features s/o Cholecystitis was seen.
Mild ascitis.
ECG-Normal study.
Blood group-O positive.
He was treated as a case of Viral pyrexia with thrombocytopenia with serositis with T2DM with left lower limb cellulitis.

Comments
Post a Comment