ACUTE PRESENTATION OF CHRONIC DIARRHOEA
Mr XYZ , a 20 year old lean Hindu boy, native of kerala, staying at chennai for his studies has been for a 1 week joyous trip with his friends somewhere in the mid february only to visit us in 1st week of March with complaints of 3-4 episodes of small volume , semisolid , bloody mucus stools. He also gives history of dyspeptic symptoms intermittently when he has oily or spicy food. He has loss of appetite, flatulence and feels tired easily these days.
He completed a 5 day course of antibiotics which are supposedly Ciprofloxacin and ornidazole. He was on probiotics for 10 days before he came to us. He says he finds no improvement in his symptoms after all the above treatment.
He says he doesn't have any abdominal pain, vomiting, nausea, black colored stools, pain while defecation, weight loss, fever, nocturnal symptoms, yellowish discolouration of skin or eyes, clay colored stools, evening rise of temperature, cough.
PAST HISTORY: No known comorbidities.
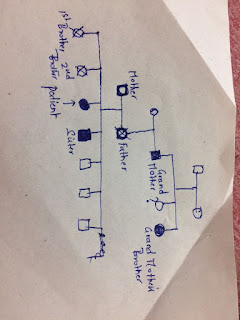
FAMILY HISTORY:
No history tuberculosis in the family.
No significant history.
PERSONAL HISTORY:
Mixed diet
Appetite reduced
Bladder regular
He doesn't consume alcohol or smoke.
GENERAL EXAMINATION:
Conscious oriented, Thin built
No pallor, icterus, cyanosis. clubbing or lymphadenopathy
Pulse - 88 bpm, regular on right radial artery, Normal volume
BP - 120/70mmhg in supine posture on both arms
RR- 16cpm
Sp02- 98% on room air
PER ABDOMEN -
Inspection: Scaphoid, No scars or sinuses
Palpation: Soft, Non tender, Liver and spleen not palpable
Percussion: No shifting dullness present.
Auscultation: Bowel sounds heard.
PER RECTAL EXAMINATION: Tone normal. Finger stained with bloody yellowish stools with mucus.
CVS- S1S2 heard, No murmurs
RS- Bilateral air entry present, Normal vesicular breath sounds.
CNS- HMF Intact, No focal neurological deficit.
WORKING DIAGNOSIS: Acute diarrhoea under evaluation-?TB Abdomen ?IBD First episode
Further we ordered certain blood investigations and imaging to rule out infectious causes of diarrhoea. Meanwhile we prescribed Rifaximin and metronidazole for 5 days and asked to review with the reports.
He came back with the following reports exactly a week later with no improvement in his symptoms.
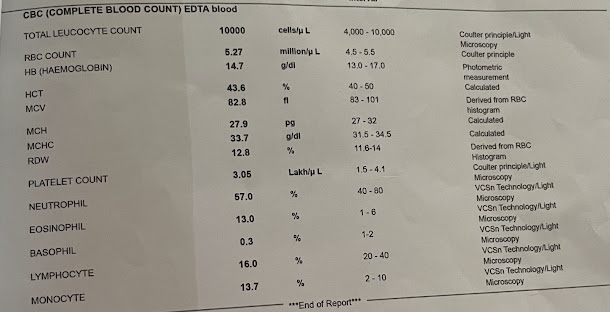
His blood investigations were normal except for CRP which was elevated.
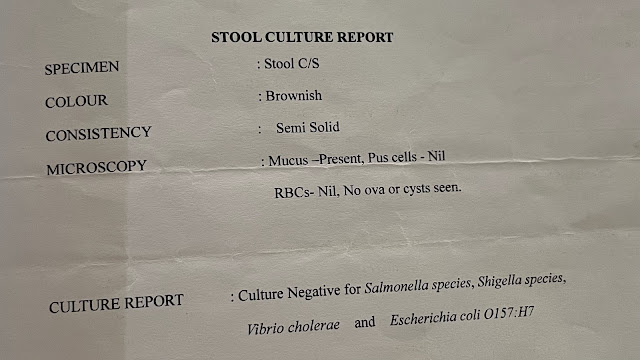
Stool examination showed Occult blood positive but was negative for infections.
He was given an option of colonoscopy thereafter and was posted for the same next day with bowel preparation.
His Colonoscopy was suggestive of INFLAMMATORY BOWEL DISEASE- SUGGESTIVE OF ULCERATIVE COLITIS.
Findings: Pancolitis (MAYO 2, UCEIS 5)
 |
HISTOPATHOLOGY REPORT: |
He was treated with Mesacol 400mg three times a day and probiotic Bifilac for 10 days and asked to review.
The next visit his symptoms improved and he was passing semisolid stools for 3 times a day. He was asked to continue the same medication for next 2 weeks.
He consumed outside food and came back with increased frequency of stools after a week and was prescribed azithromycin along with mescal and probiotic.
He came for review after a week. This time there was a drastic improvement with only 2 stools per day and no mucus. Blood in stools was noticed only on occasions.
He was prescribed Tab. Mesocal 1.2 gram twice a day with a PPI, Multivitamin and Ensure protein powder for 4 weeks.







Comments
Post a Comment